On December 13, 2024, the FDA approved cosibelimab-ipdl, a PD-L1 blocking antibody, for adults with metastatic or locally advanced cutaneous squamous cell carcinoma who are not candidates for curative surgery or radiation.
Cutaneous Squamous Cell Carcinoma
Efficacy and Safety of Cosibelimab-ipdl
The efficacy of cosibelimab-ipdl was evaluated in Study titled “Efficacy and safety of cosibelimab, an anti–PD-L1 antibody, in patients with metastatic cutaneous squamous cell carcinoma.” published on Journal of Clinical Oncology, a multicenter, multicohort, open-label trial involving 109 patients with metastatic cutaneous squamous cell carcinoma (mCSCC) or locally advanced cutaneous squamous cell carcinoma (laCSCC) who were not candidates for curative surgery or radiation. Key exclusion criteria included active or suspected autoimmune diseases, recent allogeneic transplant, prior treatment with anti-PD-1/PD-L1 blocking antibodies or other immune checkpoint inhibitors, uncontrolled cardiovascular disease, ECOG performance status ≥2, and infection with HIV, hepatitis B, or hepatitis C.
Authors: Philip R. Clingan, Daniel Brungs, Susan Arnold, Jermaine Coward, Samuel J. Fourie, Dean Laurence Harris, Andrii Kurochkin, Rahul Ladwa, Niel Malan, Andrew Michael Mant, Margie McGrath, Vinay Sharma, Hong Shue, Andrea Tazbirkova, James Oliviero, and Jayesh Desai
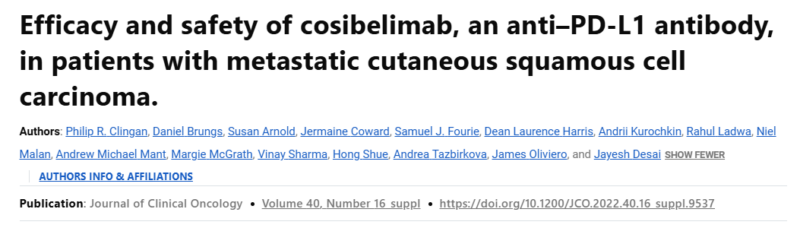
The primary efficacy endpoints were objective response rate (ORR) and duration of response (DOR), as assessed by an independent central review committee (IRC) using RECIST version 1.1. For patients with laCSCC, where externally visible target lesions were not assessable by imaging, ORR was determined by IRC assessments of digital photography (WHO criteria). The ORR was 47% (95% CI: 36-59) for patients with mCSCC (n=78) and 48% (95% CI: 30-67) for those with laCSCC (n=31). The median DOR was not reached in mCSCC patients (range: 1.4+, 34.1+ months) and was 17.7 months (range: 3.7+, 17.7 months) in laCSCC patients.
Adverse Reactions
The most common adverse reactions (≥10%) reported with cosibelimab-ipdl include fatigue, musculoskeletal pain, rash, diarrhea, hypothyroidism, constipation, nausea, headache, pruritis, edema, localized infection, and urinary tract infection. These side effects were observed in patients receiving treatment and are important considerations for monitoring and managing patient health during therapy.
The recommended dose of cosibelimab-ipdl is 1,200 mg, administered as an intravenous infusion over a period of 60 minutes, once every 3 weeks. Treatment should continue until either disease progression occurs or unacceptable toxicity is observed. This dosing schedule aims to balance therapeutic efficacy while minimizing risks associated with prolonged treatment.
This review of cosibelimab-ipdl’s safety and efficacy utilized the Assessment Aid, which is a voluntary submission from the applicant. This aid was designed to facilitate the FDA’s thorough review of the drug, ensuring that all relevant data and safety information were considered in making the approval decision.